50/M with Progressive supranuclear palsy
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Interns:
Dr Archana
Dr Sreeja
Dr Harsha
Dr Kalyan
Dr Sahithi
Dr Jeehariki
Dr Raveen PGY1
Dr Aashitha PGY2
Dr Aravind PGY3
Dr Vamshi PGY3
Dr Hareen SR
Dr Praveen Naik Ass Prof
DR. RAKESH BISWAS HOD
Here is a case i have seen:
Admission under unit 3 on 03/02/2021
Introduction:
Progressive supranuclear palsy (PSP) is a less well-known neurodegenerative brain condition which is sometimes misdiagnosed as Parkinson’s disease or Alzheimer’s.
The presence of a vertical supranuclear gaze palsy and prominent postural instability with falls in the first year of symptoms leads to a diagnosis of clinically probable PSP, and the presence of the balance disorder with slowing of vertical saccades or an isolated supranuclear gaze palsy leads to a diagnosis of clinically possible PSP.
Here we discuss a case of a 50 year old man who presented with frequently closure of eyes, frequent history of falls, tremors and self talk.
Case History:
50 year man, he presented with the complaints of
Frequently walking into objects along with frequent falls since 1.5 years
Drooping of eyelids since 1.5 years
Involuntary movements of hands since 1.5 years
Talking to self since 1.5 years
Patient works as a farmer at a local village. He completed his Inter second year. He is the father of 2 children, his elder son works as a salesman at a local company while his younger son stays at home.
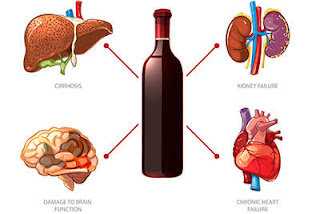
He was a regular alcoholic with daily consumption of toddy and whiskey occasionally. He also used to chew tobacco 5 - 6 times per day. He has stopped alcohol and tobacco consumption since 1 year.
10 years back, he had a sudden onset of generalised tonic clinic seizure lasting for 2 minutes after getting back from work. He was taken to a local hospital where in he got better after receiving fluids.
His wife describes him to be an aggressive individual previously and he would also throw objects in anger. She says he would often get involved in quarrels. He would get involved in matters which aren't even of his concern.
2 years back, while he was riding his bike, he had sudden blurring of vision after which he fell from his bike and attained fracture of his left leg for which he got operated. Ever since then, he says he has been having pus discharge on and off from the site of surgery.
During the hospital stay, he was told that he was a diabetic and was started on Tab Metformin 500mg once daily.
6 months after the RTA, he started finding it hard to keep his eyes open, he says it progresses as the day passes and it gets aggravated on blinking.
She says he stopped emotionally expressing himself and would not get involved in conversations with others. He started avoiding people and started being on his own.
She also says that he started talking to himself and smiling to himself since then.
He also started walking into things and he would often fall.
According to his wife and son, he only looks straight ahead while walking without looking sideways.
He also has been having involuntary movements of bilateral hands which they have noticed on and off, especially while he is doing work.
Since May 2020 he has been having non productive cough on and off, not associated with wheeze, chest pain, Dyspnea for which he visited a local hospital where in he received certain medications.
In June 2020, he visited a local hospital again because of non healing ulcer at the site of surgery.
Few days later in June, he found it difficulty to get up form his bed in the morning after which he was taken to a local hospital where in they were told that he had low levels of potassium in his blood and he was given potassium supplementation.
In the following 2 months, he continued to feel fatigued for which he visited a local hospital twice where in they were told that he had recurrent episodes of low potassium and had to be on potassium supplementation through out his life.
Over the past few months he has undergone a couple of investigations to figure out the cause of the drooping of his eyelids and sudden change in his behaviour.
Since the last 2 months, he has also been using Trihexyphenydryl 2mg twice daily.
Since the last one year, he also has been having thin stream of urine along with bed wetting at night.
On going through his old reports, he has been having a low Serum potassium of 2.5 since June and has been consistently low ever since.
In Dec 2020, it was 2.8 and in Jan 2020 it was 2.9.
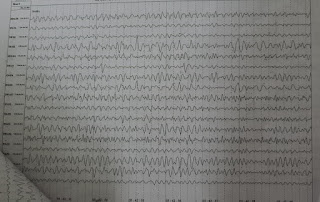
An eeg and a ct brain also was done in June 2020, which were normal
On examination:
Patient is conscious,coherent and cooperative
PR-78bpm
RR-18cpm
BP-130/70mmHg
Afebrile
Reduced arm swing 👆
CVS- S1 S2+
R/S-BAE+
P/A- Soft, Nontender
CNS Examination :
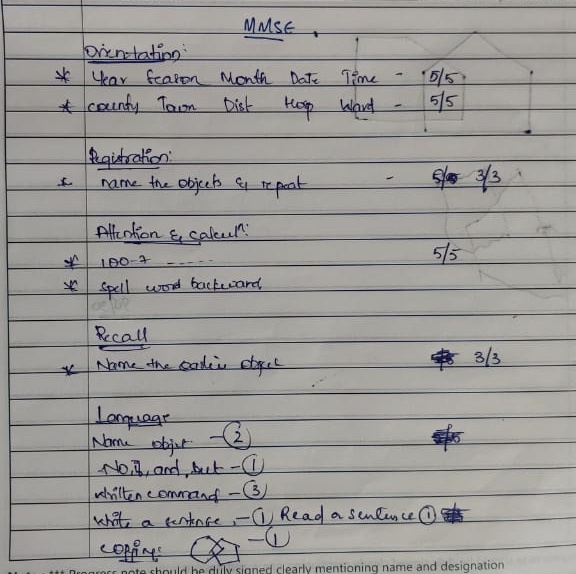
•MMSE - 30/30
•Motor system :
-Bulk- no apparent wasting
-Power- 5/5 in all 4 limbs
-Tone - increased in all the limbs
-Power - 5/5 in all the limbs
-Reflexes -
Deep tendon reflexes
Biceps -3+ in both limbs
Triceps3+ in both limbs
Supinator +in both limbs
Knee 3+ in both limbs
Ankle -rt 2+ ,left 1+
Superficial reflexes - plantars -b/l flexors
•Cranial nerves -
3rd nerve -
He is unable to perform upward gaze
ICE PACK TEST : 👆
Aim- to rule out myasthenia graves for B/L ptosis
Procedure - application of ice to the eyes for 2–5 minutes, ensuring that the ice is covered to prevent ice burns.
Result- no improvement after Ice pack test.
Inference - The results of the test can be deemed positive with a raise of 2 mm of the palpebral fissure following the removal of the ice pack. The physiological theory is by cooling the tissues, and more specifically the skeletal muscle fibres, the activity of the acetylcholinesterases are inhibited—> increased levels of acetylcholine creating the majority of the improvement.
•All other cranial nerves are intact
•Sensory system - normal
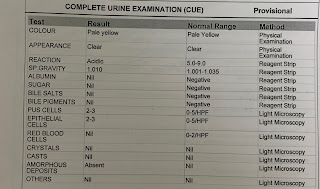
Investigations ::
CT-Brain:
EEG:
K/C/O type II DM since 2 years
Treatment :






































Comments
Post a Comment