Bimonthly assessment for the month of MARCH .
Bimonthly assessment for the month of March 2021
This is my submission for the Bimonthly internal assessment for the month of March.
The questions to the cases being discussed can be viewed in the following link :
1Q. Link to the following question :
A) What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?How specific is his dilated superficial Abdominal vein in making diagnosis?
Problem presentation :
• Fever since 15 days - not ass. with chills and rigor, intermittent type, taken medication which got relieved.
• Shortness of breath since 3 days, progressed from grade 2 to grade 4.
• Burning micturition + (duration - not given )
• No h/o palpitations, chest pain, orthopnoea, PND, pedal Edema .
No h/o cough.
Anatomical localization :
• Fever and burning micturition together suggest URINARY TRACT INFECTION
• Shortness of breath Can be due to :
1. Cardiac pathology - which is ruled out (since there is no h/o palpitations/chest pain/ orthopnoea/PND.
2. Lung pathology - can be ruled out (since there is no h/o cough or cold )
3. Liver pathology -can be due to
•abdominal distension pushing the diaphragm above.
•proteins (like albumin) synthesised by liver getting affected
—> leads to hypoproteinemia—> pulmonary oedema —> respiratory distress (SOB)
•extra hepatic manifestation of portal hypertension.
How specific is his dilated superficial Abdominal vein in making diagnosis?
• Dilated superficial abdominal veins indicate engorgement of veins - which is seen in PORTAL HYPERTENSION
Portal hypertension is an increase in the blood pressure within a system of veins called the portal venous system. Veins coming from the stomach, intestine, spleen, and pancreas merge into the portal vein, which then branches into smaller vessels and travels through the liver. If the vessels in the liver are blocked due to liver damage, blood cannot flow properly through the liver. As a result, high pressure in the portal system develops. This increased pressure in the portal vein may lead to the development of large, swollen veins (varices) within the esophagus, stomach, rectum, or umbilical area (belly button).
“ Caput medusae is one of the cardinal features of portal hypertension. The appearance is due to cutanous portosystemic collateral formation between distended and engorged paraumbilical veins that radiate from the umbilicus across the abdomen to join systemic veins. Blood from the portal venous system is shunted through the umbilical veins into the abdominal wall veins, which manifest as the caput medusae. ”
B) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? What is the cause of his hypoalbuminemia?Why is the SAAG low?
Etiology to diagnosis :
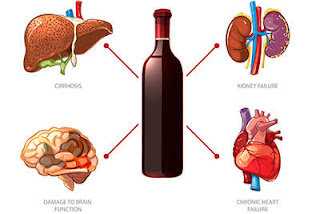
Chronic alcohol intake
🔽
Alcohol —> acetaldehyde —> NADH production
🔽
Oxidative stress
🔽
Hepatocellular injury
🔽
Cytokine production
🔽
Inflammation —> end stage = FIBROSIS = in liver = CIRRHOSIS
🔽
In cirrhosis, increased intra-hepatic resistance causes PORTAL HYPERTENSION
🔽
Patient’s SOB, Distended superficial abdominal veins.
Cause of hypoalbuminemia:
Proteins (like albumin) synthesised by liver getting affected
—> leads to hypoproteinemia
Why is the SAAG low? :
•SAAG denotes Serum Ascitis Albumin Gradient :
• low SAAG
—> less of serum albumin, more of a Ascitis albumin —> EXUDATE type of Peritoneal Paracentesis :
local causes like TB, malignancy
c)Will PT,INR derangement preceed hypoalbuminemia in liver dysfunction??Share reference articles if any!
It can occur, in a patient who already has sepsis—> extensive endothelial damage—> deranged coagulation profile
“ The liver is responsible for the synthesis of many of the procoagulant and anticoagulant proteins responsible for maintaining hemostasis.17 Liver dysfunction is often assumed to be associated with increased bleeding risk, but evidence suggests that other factors such as sepsis, hepatorenal syndrome, hypotension, and endothelial dysfunction contribute to this bleeding tendency rather than isolated cirrhosis and liver disease. ”
d)What is the etiology of his fever and pancytopenia?
e)Can there be conditions with severe hypoalbuminemia but no pedal edema? Can one have hereditary analbuminemia and yet have minimal edema? Please go this article https://www.
Yes
Inflammation and infection
Albumin is considered a negative acute phase reactant, which means that as inflammation and other acute physiologic processes occur, its levels decrease
In liver disease:Albumin is synthesized in the liver, and low serum albumin can be indicative of liver failure or diseases such as cirrhosis and chronic hepatitis. If present, hypoalbuminemia is generally considered to be a sign of advanced hepatic cirrhosis, or irreversible damage to the liver
Malnutrition or malabsorption
Low albumin levels can also indicate chronic malnutrition from protein losing enteropathy.[3] This is often caused or exacerbated by ulcerative colitis,[10] but can also be seen in cardiac disease and systemic lupus erythematosus.
Conditions with severe hypoalbuminemia and no pedal edema- There can be a compensatory synthesis of protiens (globulins) other than albumin and thereby maintain the oncotic pressure in the intravascular compartment and preventing the extravasation of fluid. This could also be possible if there is a hypovolemic state in the same patient with hypoalbuminemia so that the pressures are again maintained and there is no fluid accumulation.
It is possible for one with hereditary analbuminemia to not have pedal edema. Since it is a chronic and hereditary disease there can be compensatory synthesis of other plasma proteins.
f) What is the efficacy of each of the drugs listed in his current treatment plan
Ans: tamsulosin efficacy in UTI patients
1.α1-Adrenergic receptor antagonists are used by 80% of physicians as the first agent to treat patients with benign prostatic hyperplasia (BPH) presenting with lower urinary tract symptoms (LUTS); 27 of 30 clinical trials have confirmed that α-blockers are effective for BPH treatment.
2.Tamsulosin's α1A subtype adrenergic receptor selectivity is considered to be responsible for its low cardiovascular side effects and lack of interaction with antihypertensives.
3.A 4-year extension, multicenter, open-label, phase IIIB clinical study evaluated long-term efficacy, safety, and tolerability of tamsulosin for up to 6 years; the study found a consistent statistically significant improvement in AUA symptom scores over 6 years, and most patients showed improvement during the first year that was sustained over 6 years.
4.The low incidence of acute urinary retention in patients treated with tamsulosin for up to 6 years suggests that tamsulosin may reduce the risk of AUR in patients with BPH.
5.Response to treatment and incidence of adverse events (eg, rhinitis and abnormal ejaculation) in patients with hypertension, diabetes, or nonhypertensive cardiovascular disease did not differ significantly from that in those without.
6.Abnormal ejaculation is an important side effect of tamsulosin, but it resulted in few discontinuations during treatment. It may not always be deemed important by patients, and was not linked to complaints of decreased libido, impotence, or other changes in sexual function.
Nitrofurantoin efficacy:
comparing 3 days of nitrofurantoin with placebo in young women with symptoms of UTI and pyuria found clinical cure rates of 70% versus 42%, respectively, 7 days after the start of therapy.
The prevalence of participants with side effects attributed to nitrofurantoin in the 17 studies generally ranged from 5% to 16%; nausea, abdominal discomfort and headaches were described. An exception was an open-label randomized controlled trial whose primary outcome was quality of life.
QUESTION 2
45year old female with abdominal distension
https://navyamallempalli.blogspot.com/2021/02/dr_6.html
a). What is the problem representation of this patient and what is the anatomical localization for her current problem based on the clinical findings?
PROBLEM REPRESENTATION:
1.Abdominal distension since 2years
2.shortness of breath
3.pedal edema since 2 months
4.cachexia_malnourishment
Anatomical localisation:
1.abdominal distension : causes: fluid,fetus,flatus,fat,feaces
Here in this case:
O/E: flankfullness and fluid thrill is present __indicates distension is because of fluid_ASCITIS
In this case the pattern is ascitis followed by pedal edema _clinically it indicates problem is in liver.
2.shortness of breath and dull note in right side _IAA,ISA,IMA and decreased breath sounds on right side indicates pleural effusion .most likely in this case pleural effusion is due to her refractory ascitis _HEPATIC HYDROTHORAX.
3.Cachexia _ is due to her loss of appetite which in turn because of massive ascitis .
Overall the major problem in this case_refractory ascitis since 2 years.
b) What is the etiology of her refractory ascites and pleural effusion? and how would you as a member of the treating team arrive at a diagnosis?
Ans:
In this case ,ascitis recurs shortly after therapuetic paracentesis despite sodium restriction and diuretic treatment._refractory ascitis.
CAUSES OF REFRACTORY ASCITIS:
1.Non compliance to treatment
2.Tumor_hepatoma
3.Renal failure
4.spotaneous bacterial peritonitis
5.Portal vein thrombosis
6.NSAIDS
7.Infection
8.GI Bledding
On ascitic fluid analysis: It is high SAAG and low protein ,it probably due to portal hypertension.
she is on diuretics,frequent therapeutic paracentesis
Her RFT was normal _no renal failure,
Noincreased cell counts in ascitic fluid, no features of infection _rule out SBP
No H/O 7se of NSAIDS
On CECT abdomen_ no tumors identified in liver
No symptoms of GI bleeding:melena,hemetemesis.
So in this case most probably ascitis due to portal hypertension :
DD: cirrhosis of liver
Schistosomiasis
Portal vein outflow obstruction.
Cirrhosis is ruled out clinically no symptoms like jaundice,no coagulation disorders,no other signs of liver cell failure radiologically no altered echotexture,no shrunken liver,no nodules .
Stool microscopy was done to rule out schistosomiasis.
Portal vein thrombosis evaluation done by triple phase cect followed byMR Venogram.
On triple phase CECT :Focal short segment of intrahepatic segment of IVC just below the diaphragm with normal hepaticveins And multiple osteosclerotic lesions in pelvis,ribs,vertebral bodies __sarcoidosis /metastasis.
MR Vengram_ suggested severe narrowing of intrahepatic portion of IVC___Chronic buud chiari syndrome.
PLEURAL EFFUSION:
When pleural and Ascitic tap done on same time sent for analysis _both looks like almost same _both are transudates:so, pleural effusion is most likely due to Hepatic hydrothorax.
DD: 1.sarcoidosis:
2.tuberculosis: pleural fluid and sputum for AFB and CBNAAT was negative.clinically no h/o TB.
3.Malignancy: pleural fliuid cytology was normal ,no dysplastic cells
c) Approach to a patient with ascites?Clinically is there any way to differentiate pre hepatic, post hepatic and hepatic causes?
d)Causes of budd chiari syndrome?Why did the patient undergo bone biopsy?
Hypercoagulable states:
Inherited : Anti thrombin deficiency, Protein c deficiency,protein S deficiency,Factor v leiden mutation, prothrombin mutation
Acquired :Myeloproliferative disorders,PNH,Anti phospholipid syndrome,cancer,pregnancy,ocp use
Uncommon causes: HCC,RCC,Adrenl carcinoma
Misc: Aspergillosis,behcet syndrome,IVC webs,trauma,IBD,systemic sarcoidosis.
IN THIS CASE BONE BIOPSY DONE FROM POSTERIOR ILIAC CREST ON LEFT SIDE TO EVALUATE THE OSTEOSCLEROTIC LESIONS IN PELVIS , RIBS, VERTEBRAE .
d) Management strategies for refractory ascites and Budd chiari syndrome? Share the potential advantages and disadvantages of Peritoneal dialysis catheter placement in refractory ascites?
Ans:
Management of BCS:
1.Diagnosis of BCS made by clinical features, laboratory and radiological investigations , management of underlying cause
2.Anti coagulant therapy with LMWH and then warfarin aim for INR 2_3
3.Treat the complications of portal hypertension with spirinolactone ,furosemide,and gastroscopy for variceal screening and band ligation
4.consider angioplasty /stenting for venous obstruction
5.consider TIPS if no improvement with anticoagulation , angioplasty, stenting.
6.TIPS fails /no improvement and acute liver failure consider liver transplantation.
7.Monitor chronic BCS for HCC by 6 monthly USG and alpha fetoprotein.
Management of refractory ascitis :
Peritoneal dialysis catheter in refractory ascitis:
Advantages:
Heamodynamic stability
Ascitis control directly and in continuing fashion
Easy catheter placement
Disadvantages:
Protein loss
Over drainage of ascitis lead to hypotension
Dialysate leak or hydrothorax
Poor clearance owing to volume of ascitis
Higher infection risk .
https://clinicaltrials.gov/ct2/show/NCT02975726
e) What is the efficacy of each of the drugs listed in his current treatment plan
Lasilactone
https://www.medicines.org.uk/emc/product/907/smpc
Warfarin and LMWH:
https://emedicine.medscape.com/article/184430-medication
f)What is the current outcome?and what could be the etiology of her current outcome?
Ans:
Patient got expired on14th of march preceded h/o vomiting and nausea
Cause of death was not confirmed, may be because of dislodgement of thrombus leading to pulmonary embolism.
QUESTION 3
55year old male with SOB and abdominal distension,orthopnea
https://jayanth1802.blogspot.com/2021/02/55-year-old-farmer-with-sob-abdominal.html?m=1
a). What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
-Based on the clinical findings the problem in this patient is with his heart.
Based on the detailed history and clinical findings the provisional diagnosis would be- k/c/o cor pulmonale with severe pulmonary arterial hypertension grade III with gross ascitis with acute kidney injury.
b) What is the etiology of his ascites? and how would you as a member of the treating team arrive at a diagnosis?Chart out the sequence of events!
-The reason for ascitis in this patient could be RHF. RHF leads to congestive hepatomegaly and thereby derranging the synthetic funtion of the liver to produce albumin. And hypoalbuminemia leads to fluid accumulation.
AKI can also lead to ascitis due to increased salt and water retention.
COPD
---->RHF
----> congestive hepatomegaly
----> reduced protein synthesis
----> ascitis due to fluid accumulation.
Decreased urine output
--->AKI
---> Salt and water retention
----> ascitis.
c)What is the efficacy of each of the drugs listed in his treatment plan?
LASIX (FUROSEMIDE) in congestive heart failure:
“ diuretics used are furosemide, bumetanide and chlorothiazide. The available data from several small controlled trials show that in patients with CHF, conventional diuretics appear to reduce the risk of death and worsening heart failure when compared to an inactive sugar pill (placebo). About 80 deaths may be avoided for every 1000 people treated. Diuretics also increase the ability to exercise, by about 28% to 33% more than with other active drugs. These conclusions were based on 14 controlled trials (525 people), of which three trials noted deaths in 202 people randomised to receive either diuretic or placebo, and two trials, a total of 169 people, looked at hospitalisation for worsening heart failure. Of the seven trials comparing diuretic treatment with another drug, the effects on exercise were studied in four trials where 91 people were randomised to receive either a diuretic or an ACE inhibitor or digoxin. Most of the trials had small numbers and lasted from 4 to 24 weeks, a short time for a chronic disease. The age of the participants was 59 years, which is relatively young, and the use of diuretic drug was not standardised across the studies. More research would be needed to further confirm the long term benefits of diuretic treatment for CHF patients because these studies were small.”
d)What are his current outcomes ?
- The patient can go in cardiopulmonary arrest.
QUESTION 4
4)Please go through the thesis presentation below and answer the questions below by also discussing them with the presenter
https://youtu.be/QlPrb1BSHGE
a)What was the research question in the above thesis presentation?
-Role of SAAG in diagnosing the etiology of ascitis.
b) What was the researcher's hypothesis?
41/F, with retro virus positive, c/o : abdominal distension (duration ?) , fever— was diagnosed as ascitis secondary to Chronic liver disease.
First they thought the ascitis maybe secondary to TB (TUBERCULAR PERITONITIS) .
🔽
Peritoneal Paracentesis is performed, SAAG was expected to be low, but the result of SAAG, took a 360 degree turn in diagnosing the patient.
🔽
SAAG RESULT came out HIGH, after which they suspected ART (anti retro-viral therapy) INJURY TO HEPATOCYTES leading to CHRONIC LIVER DISEASE
c)What is the current available sensitivity and specificity of SAAG in diagnosis of etiology of ascites
When using the SAAG cut-off value 11 g/L, its sensitivity and specificity were 100.00% and 85.19% with an accuracy of 94.37%.
https://diagnosticpathology.biomedcentral.com/articles/10.1186/1746-1596-8-143#:~:text=When%20using%20the%20SAAG%20cut,%25%2C%20P%3C0.01).
Question 5 :
5) Journal club questions on Ascites theme
Please identify the study design and outcomes in the article linked here https://www.ncbi.nlm.nih.
STUDY DESIGN
Institution-based cross-sectional study.
THESIS IS ABOUT:
CLINICAL PROFILE,EVALUATION,DIAGNOSIS AND THERAPEUTIC OUTCOMES IN PATIENTS WITH ASCITES
STUDY DESIGN
Prospective study, Qualitative, Non Experimental









Comments
Post a Comment