Bimonthly assessment for the month of feb 2021
1Q. 50 year man, he presented with the complaints of
Frequently walking into objects along with frequent falls since 1.5 years
Drooping of eyelids since 1.5 years
Involuntary movements of hands since 1.5 years
Talking to self since 1.5 years
a. What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
This is our unit case, and I’ve got the opportunity to prepare the blog for this. I’ve read about Parkinsonism plus syndrome in my final year MBBS, and seeing one i.e., PROGRESSIVE SUPRANUCLEAR PALSY, added a whole new perspective to my theory knowledge.
Problem presentation :
50 year old male, presented with the complaints of:
• Frequently walking into objects along with frequent falls (especially on climbing upstairs) since 1.5 years
• Drooping of eyelids since 1.5 years
• Involuntary movements of hands since 1.5 years
• Talking to self since 1.5 years
He had reduced arm swing and emotionless face (mask like)
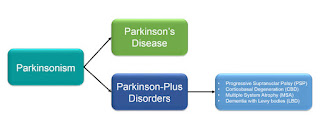
The above features fits into Parkinsonism plus syndrome.
Localisation of lesion :
1.Frequent falls on walking (especially climbing upstairs) :
• 🚩 vertical gaze palsy : as the patient is having problem on moving his eyeball up and down, falling while climbing stairs (for which upward movement of eyeball is needed) is affected, vertical gaze is affected especially in PROGRESSIVE SUPRANUCLEAR PALSY.
2. Drooping of eyelids in both eyes:
Called as bilateral ptosis.
Elevators of upper eyelid are :
• 🚩levator palpebrae superioris - supplied by oculomotor nerve —>arising from midbrain—> if affected, causes >2mm ptosis
• 🚩Muller's muscle - supplies by sympathetic nerve supply —-> if affected, causes 2mm ptosis
3. Involuntary movements ( tremors ) in upper limbs:
• 🚩basal ganglia if affected—> inhibition is lost—> resulting in tremors.
Other types of tremors are 👇
4. Talking to self :
•🚩Pre-frontal lobe lesion ( which has decision making, personality expression, Moderates social behaviour)
As multiple areas of brain are involved, it suggests NEURODEGENERATIVE DISEASE.
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
I came across two differentials involving this case.,
1. OCULAR MYASTHENIA GRAVIS : since the patient complained about ptosis progressing as the day progressed. We performed “Ice pack test” with the help of ophthalmology department, but there was no improvement in ptosis, by which I ruled out ocular myasthenia gravis.
2. PARKINSONISM PLUS SYNDROME ( PROGRESSIVE SUPRANUCLEAR PALSY):
• Since the patient had trouble in shifting the gaze in vertical direction, resulting in frequent falls on climbing stairs.
• angry outbursts, leading to throwing objects at anyone and no one.
• Facial apathy (mask like face).
Sequence of events:
Habitual alcohol drinker since 30years (stopped 1 year back), habitual smoker since 30 years (stopped 1 year back)
|
Seizures 10 years back
|
Type 2DM 2 years back
|
Sudden blurring of vision while riding bike met with RTA —> fracture in left leg, operated 2 years back
|
Frequently walking into objects along with frequent falls, drooping of eyelids, Involuntary movements of hands, Talking to self since 1.5 years.
|
Non healing ulcer at surgical site 7 months back (post implant failure)
|
Diagnosed as PSP & discharged with SYNDOPA 110mg & QUETIAPINE in kamineni, narketpally
1 month back
|
5 days later, patient presented to casualty in a state of unresponsiveness with GCS: 3/15 with H/o 2-3 episodes GTCS seizures.
Another 2 episodes of generalized tonic seizures in casualty - treated with levipil
Suddenly his saturations & heart rate dropped with no peripheral pulsations and patient was intubated - CPR done and was resuscitated.
Patient was put on mechanical ventilator - CPAP mode.
Later, weaning was done, GCS improved to 8/15.
Patient is still in ICU, and his vitals are monitored hourly.
c) What is the efficacy of each of the drugs listed in his current treatment plan
Patient was put on SYNDOPA and QUETIAPINE:
Currently no medication is known to be effective in PSP. Currently, PSP patients are prescribed medications used in Parkinson’S disease. Only few subjects responded, but the effect is minimal.
Efficacy of Syndopa in the following link 👇
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2699657
Efficacy of Quetiapine in the following link 👇
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2699657/
2Q. Patient was apparently asymptomatic 2 years back then he developed weakness in the right upper and lower limb, loss of speech.
a) What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
Problem representation:
A 60 year old man with a history of CVA 6 months back presented with
• Weakness in right upper and lower limb with loss of speech 2 years back.
•Shortness of breath since 2 months (grade 2 progressed to grade 4 ( on rest) with orthopnea and paroxysmal nocturnal dyspnea. )
•Bilateral pedal edema since 2 months
•Reduced urine output since 2 months
•Generalised weakness since 2 months
Anatomical localization :
•🚩 Localization is at the level of heart, secondary to atherosclerosis of vessel .
•🚩History suggests SOB grade 2 to 4 (even on rest), orthopnea and paroxysmal nocturnal dyspnea.
Classical symptoms of left heart failure.
Examination findings -
•🚩Apex beat at 6th ICS - probably because of ventricular hypertrophy apex beat being displaced.
•🚩Pedal edema upto knee which is Grade 2 ---maybe because the patient might have developed features of RIGHT HEART FAILURE too, due to back pressure.
•Loud p2
•🚩 Bilateral fine Crepitations present in axillary,infra axillary and infrascapular areas —> can indicate PULMONARY EDEMA, which is due to left heart failure—> back pressure to pulmonary veins
—> back pressure to alveoli.
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
Etiology:
CAD leading to DCMP
ECG showing :
1)normal axis
2)pathological Q waves from v1 to v6 (pathological Q waves = more than 1/3 rd of R wave)
3)poor R wave progression
suggest a CAD probably involving LAD and LCX
Etiopathogenesis :
Alcohol overintake
🔽
Deranged lipid profile
🔽
Atherosclerosis of vessels
🔽
Affecting coronary vessels
🔽
Myocardial infarction
Source:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2365733/
Sequence of events :
CVA—2 years back
and
SOB, pedal edema, decreased urine output & generalized weakness since 2months
and
Treated with diuretics(aldosterone antagonist) and beta blockers ,ARB
With salt and Fluid restriction.
Outcome: Symptomatically improved and discharged
c) What is the efficacy of each of the drugs listed in his current treatment plan ?
1: Salt and fluid restriction :
Individualized salt and fluid restriction can improve signs and symptoms of CHF with no negative effects on thirst, appetite, or QoL in patients with moderate to severe CHF and previous signs of fluid retention.
Source:
https://pubmed.ncbi.nlm.nih.gov/23787719
2)Spironolactone
One study has shown that spironolactone improves morbidity and mortality in patients with severe heart failure. The particular advantages of spironolactone for prevention are that it is inexpensive, is taken once daily and has relatively few side effects. This study suggests that all patients with class IV heart failure should be given a trial of spironolactone.
Source:
3)Benfomet as thiamine replacement in alcoholic pts:
Benfomet appears to reduce psychiatric distress and may facilitate recovery in severely affected males with lifetime alcohol dependence and should be considered for adjuvant therapy in alcohol rehabilitation.
Source : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4550087/
4) Furosemide :
Diuretics effectively treat the sodium and water retention found in the syndrome of heart failure. When given intravenously, the loop diuretic frusemide brings about rapid symptomatic relief, an effect preceding the increase in urinary sodium and water output by up to 30 min.
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2014966/
3Q. 52 year old male , shopkeeper by profession complains of SOB, cough ,decrease sleep and appetite since 10 days and developed severe hyponatremia soon after admission.
Case presentation video:
a) What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
Problem representation:
A 52 year old man, who is a known to be a Diabetic and hypertensive presented with:
• Dyspnea since 10 days
• Productive cough since 2 days
• Disturbed sleep since 10 days
Anatomical localization:
The anatomical location of the problem is in the lungs (since grade 2/3 SOB without palpitations/chest pain/PND/orthopnoea can be attributed to lung problem)
Lower respiratory tract infection
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
No respiratory examination has been mentioned in the elog.
However his problems list are:
- Hyponatremia (seen in the report of RFT)
-Lower respiratory tract infection(on history)
-Uncontrolled blood sugars ( seen with the help of GRBS charting)
-Dimorphic Anemia
(Based on history --
Sob 2 to 3,generalized weakness, decreased appetite (anemia causing heart failure)
O/E - on examination of lower palpbreal conjuctiva -pallor+
Peripheral smear - microcyte/ + macrocytes, hypersegmented neutrophils are present )
Sequence of events
52 year old with DM Type 2 and HTN
🔽
Developed symptoms of sob, cough, decrease in sleep and appetite, generalized weakness
🔽
Patient developed anemia (most common cause of anemia is NUTRITIONAL ANEMIA) with uncontrolled blood sugars.
⬇️
Hyponatremia (blood sodium levels = 121 mEq/L) came as an incidental finding. Patient developed drowsiness because of movement of water into the cell leading to CEREBRAL EDEMA.
🚩Our treatment team initially sent a urinary sodium and serum electrolyte sample
to differentiate between types of hyponatremia.
🚩 First -restricting fluids with minimal intake of hypertonic saline 3%
🚩Calculation of the sodium deficit:
0.6 x weight(kg) x (desired Na+ - Actual Na+). Use 0.5 for females. Desired Na+= 120-125 meq/l.
Example: 70kg male. Na+= 110 meq/l Desired target= 125 meq/l.
[0.6 x 70kg x (125-110)= 630 meq of Na+ needed].
Amount needed to increase serum sodium level by 1 meq/l/hr= 0.6 x 70kg x 1.0= 42 meq/hr (safe rate for this patient).
3%--hypertonic saline contains 513 meq/liter.
Therefore: [desired rate per hr] / 513 x 1000 = infusion rate (ml/hr).
And the total infusion time= [total meq needed] / [meq/hr]
Desired rate= 42/513 meq x 1000= 82 ml/hr
Infusion time= [630 meq] / [42 meq/hr] = 15 hrs.
Therefore: Infuse 3% saline at 82 ml/hr for 15 hours.
Source-
 https://globalrph.com/dilution/sodium-chloride/
•Maximum correction for Na which can corrected in a day is 8-10 meq
•First 4 hrs -4meq has to be corrected
•Next 20 hrs -remaining calcuated Na should be given
•we have to control sugars since for every 100mg increase in sugars, 1.6 Na will decrease (remembered as sweet 16)
However in a type 2 diabetic we consider 124 too as normal Na range
Source of the above points =2-4 Class
2) proper control of sugars with insulin and metformin
c) What is the efficacy of each of the drugs listed in his current treatment plan especially for his hyponatremia? What is the efficacy of Vaptans over placebo? Can one give both 3% sodium as well as vaptan to the same patients?
Answer--
1) Efficacy of vaptans over placebo :
https://acsjournals.onlinelibrary.wiley.com/doi/full/10.1002/cncr.28468
2) Can one give both 3% sodium as well as vaptan to the same patient?
No,
We shouldn't give both at a time.
Since there is a risk of over correction leading to hypernatremia.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5752787/
4) Please mention your individual learning experiences from this month.
I’ve seen cases that are very rare, like:
1. Progressive Supranuclear Palsy
2. Incidental finding of Hyponatremia in a patient that came with chief complaint of SOB, and later presented with drowsiness.
3. Psychogenic polydipsia leading to Hyponatremia.
I’ve seen many cases with :
• Heart failure ( I’ve heard pansystolic murmur. )
• COPD patients
• Alcohol dependance syndrome with tremors, alcoholic liver disease
• Acute on chronic pancreatitis patients.
• Diabetic Ketoacidosis
• hemiparesis cases
I’ve prepared blogs for some of my patients admitted :
1. 34/M with right sided hemiplegia
2. 30/M with Polyarthralgia :
3. 43/M with Pancreatic Pseudocyst
4. 50/M with PSP
5. 30/M with epigastric pain
Ive learnt many clinical points in morning rounds :
•🚩Erythema multiforme labialis: due to drug reaction
•🚩Scraping of tongue—> transporting it in a sterile container—> on KOH Mount, budding yeasts and hyphae seen, suggesting CANDIDA
•🚩I’ve seen a case with MELENA, whose stool microscopy (which I’ve seen the microbiologist preparing the stool sample) showed plenty of pus cells.
•🚩Deep jaundice :
I’ve taken videos of case presentation and case discussion in 2-4 pm session, and uploaded them on YouTube .
I’ve done diagnostic ascitic tap for a nephrotic syndrome patient with ascitis.
I enjoyed the interactive sessions with my professors and my pg’s :












Comments
Post a Comment